Behandlungsablauf
Das erste Gespräch
An Ihrem ersten Termin im HIT werden Sie mit dem für Ihre Behandlung zuständigen Facharzt für Strahlentherapie ein ausführliches Gespräch führen. Dieser bespricht mir Ihnen Ihre Erkrankung und klärt Sie genauestens über die Wirkung der Ionenstrahltherapie auf. Selbstverständlich nimmt sich Ihr Arzt auch Zeit für alle Ihre Fragen.
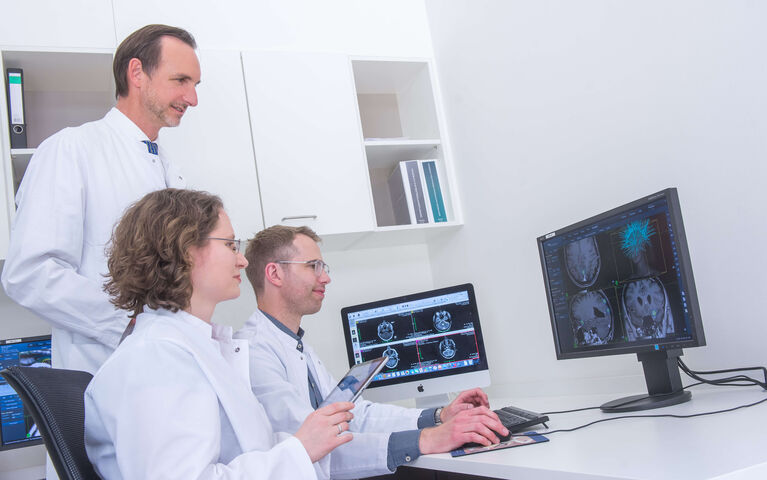
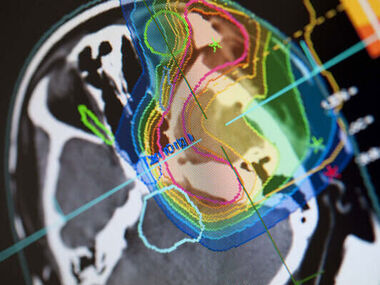
Die Strahlentherapie-Planung
Bevor es mit Ihrer ersten Bestrahlung am HIT losgeht, findet zunächst eine individuelle Strahlentherapie-Planung statt. Die Behandlung kann nur dann erfolgreich sein, wenn der Therapiestrahl den Tumor zielgenau trifft.
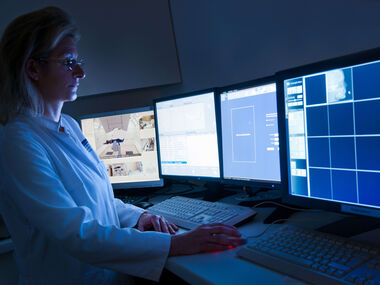
Um die Umrisse des Tumors mit höchster Genauigkeit zu ermitteln werden spezielle bildgebende Verfahren, wie Computer- oder Magnetresonanztomographie eingesetzt. Innerhalb von Sekundenbruchteilen wird eine dreidimensionale Computersimulation des Tumors und seiner Umgebung auf dem Bildschirm dargestellt. Die Ärzte geben dann bestimmte Werte vor, z.B. die Konturen des Tumorvolumens und seine räumlichen Koordinaten, die Solldosis im Tumor und die Toleranzdosen des gesunden Nachbargewebes. Daraus berechnet der Computer die optimale Strahlendosis für jeden einzelnen Punkt im Tumor und ermittelt die günstigsten Einstrahlrichtungen des Therapiestrahls.
Genaue Positionierung
Damit es durch Bewegungen des Körpers nicht zu Ungenauigkeiten kommt und der Tumor auch bei mehreren aufeinander folgenden Bestrahlungen in exakt der gleichen Position bestrahlt werden kann, stellen wir für Sie individuell angepasste Lagerungshilfen her. Je nachdem welcher Körperbereich bei Ihnen bestrahlt werden soll, kommen unterschiedliche Hilfsmittel zum Einsatz. Beispielsweise sind das nach Maß angefertigte Kunststoffmasken für die Bestrahlung im Kopf-Halsbereich.
Die Behandlungsräume
Die technische Ausstattung des HIT garantiert den Patienten eine Strahlentherapie auf international höchstem Niveau. Zwei Behandlungsräume sind mit einem festen, horizontalen Strahl ausgestattet, der aus der Wand austritt. Hier kommt auch unser mobiles Airo CT-Gerät zur 3D-Bildgebung zum Einsatz, mit dem eine Lagekontrolle direkt im Behandlungsraum durchgeführt und eine adaptive Bestrahlung ermöglicht werden kann. Im dritten Behandlungsraum befindet sich die weltweit erste Schwerionen-Gantry, eine bewegliche Strahlenquelle, die 360° um den Tumor rotieren und verschiedene Einstrahlrichtungen einnehmen kann. Die Behandlungstische sind in drei Richtungen, sowie drei Rotationen beweglich und werden robotergesteuert in die vorher berechnete optimale Position gefahren. Röntgengeräte und Sensoren prüfen vor und während der Bestrahlung die Genauigkeit der Positionierung und der Bestrahlung. Dies ist die weltweit präziseste Positionierung eines Patienten unter der Bestrahlungsquelle.
Die Bestrahlung
Ein wenig Lampenfieber vor der ersten Bestrahlung ist verständlich, aber unbegründet. Die Bestrahlung ist völlig schmerzlos und dauert bei den meisten Patienten nur 30 Sekunden bis wenige Minuten. Um jede einzelne Tumorzelle zu zerstören sind mehrere aufeinander folgende Bestrahlungen notwendig. Die Bestrahlungspausen werden so gewählt, dass sich mitbestrahltes gesundes Gewebe erholen und seine Strahlenschäden reparieren kann. Krebszellen schaffen das nicht so schnell. Daher addieren sich im Tumor die Strahlenschäden der einzelnen Bestrahlungen und zerstören ihn schließlich. Die gesamte Bestrahlung besteht aus durchschnittlich 20 Einzelbestrahlungen. Fast 90 Prozent unserer Patienten werden ambulant bestrahlt, das heißt, sie können nach der Bestrahlung nach Hause gehen.
Mehrere Wochen nach den Bestrahlungen kontrollieren die Ärzte mit CT oder MRT, ob der Tumor kleiner geworden oder sogar ganz verschwunden ist.