Wabnitz Lab
Granulocyte Biology in Health and Disease
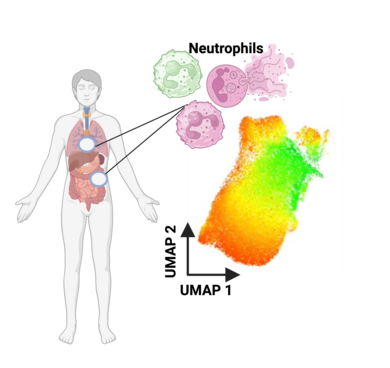
Neutrophils, the most abundant granulocytes, are first responders in immune defense, combating infections through phagocytosis, degranulation, and NET formation. Beyond their protective role, they contribute to tissue homeostasis by regulating inflammation and interacting with other immune cells. Dysregulation, however, can lead to chronic inflammation, autoimmunity, or impaired host defense. Recent advances in neutrophil biology reveal their heterogeneity and plasticity, offering insights into their dual roles in health and disease. Understanding these versatile cells is crucial for developing targeted therapies in inflammatory and autoimmune disorders.
Focus 1: Neutrophil Phenotypes Across Inflammatory Landscapes
Polymorphonuclear neutrophil granulocytes (PMNs) are the most abundant leukocytes in human blood, with a short lifespan of only a few hours in circulation. However, once they migrate into tissues, their lifespan is extended by signals from the local microenvironment. These signals drive neutrophil diversification, altering their phenotype and functions to adapt to specific tasks such as infection defense or wound healing. While essential for immune response, diversified neutrophils can also contribute to tissue damage, particularly in chronic inflammatory diseases.
Our research focuses on understanding how CCR5+ neutrophils, a pro-NETotic subset, respond to different microenvironments. These neutrophils are known for their ability to form neutrophil extracellular traps (NETs), a mechanism that can exacerbate inflammation and is implicated in rheumatoid arthritis (RA) and ulcerative colitis (UC). In these diseases, the overactive neutrophil responses contribute to ongoing tissue damage and chronic inflammation, further complicating the disease pathology.
We aim to explore how neutrophils sense and interpret their microenvironment to induce phenotypic and functional changes, and to investigate whether certain neutrophil phenotypes are characteristic of specific diseases. Moreover, we are interested in understanding how diversified neutrophils modulate T cell-mediated immunity, which plays a critical role in chronic inflammatory conditions. By uncovering these interactions, we hope to pave the way for novel diagnostic and therapeutic strategies to better manage chronic inflammatory diseases where neutrophil-driven pathology is central.
Focus 2: Immune Dimensions of Dilated Cardiomyopathy
Dilated Cardiomyopathy (DCM) is a condition characterized by the enlargement and impaired function of the heart's ventricles, leading to weakened heart performance and potentially heart failure. We are investigating the immune landscape of DCM patients to uncover the role of immune cells, particularly T cells and neutrophils, in disease progression. Through advanced techniques such as single-cell transcriptomics and immune phenotyping, we aim to better understand the shifts in immune cell populations, as well as markers of chronic inflammation, that may contribute to fibrosis and cardiac dysfunction. These insights could pave the way for new therapeutic approaches in DCM management.
Research team
Anna Makari (cand. MD, PROMOS Stipendium)
Julia Cygan (cand. MD)
Amelie Bauerdick (cand. MD / Otto-Hess-Promotionsstipendium)
Franz Kahlich (cand. MD)
Jüri Habicht Lab coordinator (MTA)
Publications
Neuenfeldt F, Schumacher JC, Grieshaber-Bouyer R, Habicht J, Schröder-Braunstein J, Gauss A, Merle U, Niesler B, Heineken N, Dalpke A, Gaida MM, Giese T, Meuer S, Samstag Y, Wabnitz G. Inflammation induces pro-NETotic neutrophils via TNFR2 signaling. Cell Rep. 2022; 39, 110710
Grieshaber-Bouyer R, Exner T, Hackert NS, Radtke FA, Jelinsky SA, Halyabar O, Wactor A, Karimizadeh E, Brennan J, Schettini J, Jonsson H, Rao DA, Henderson LA, Muller-Tidow C, Lorenz HM, Wabnitz G, Lederer JA, Hadjipanayis A, Nigrovic PA. Ageing and interferon gamma response drive the phenotype of neutrophils in the inflamed joint. Ann Rheum Dis. 2022;81(6);805-814.
Wabnitz GH, Honus S, Habicht J, Orlik C, Kirchgessner H, and Samstag Y. LFA-1 cluster formation in T-cells depends on L-plastinphosphorylation regulated by P90(RSK) and PP2A. Cell Mol Life Sci. 2021;78(7):3543-64.
Wu, J., Ma, S., Sandhoff, R., Ming, Y., Hotz-Wagenblatt, A., Timmerman, V., Bonello-Palot, N., Schlotter-Weigel, B., Auer-Grumbach, M., Seeman, P., Loscher, W. N., Reindl, M., Weiss, F., Mah, E., Weisshaar, N., Madi, A., Mohr, K., Schlimbach, T., Velasco, Cardenas, R. M., Koeppel, J., Grunschlager, F., Muller, L., Baumeister, M., Brugger, B., Schmitt, M., Wabnitz, G., Samstag, Y., Cui, G. Loss of Neurological Disease HSAN-I-Associated Gene SPTLC2 Impairs CD8+ T Cell Responses to Infection by Inhibiting T Cell Metabolic Fitness, Immunity, 2019 May 21;50(5):1218-1231.e5.
Wabnitz GH, Kirchgessner H, Jahraus B, Umansky L, Shenolikar S, and Samstag Y. Protein Phosphatase 1alpha and Cofilin Regulate Nuclear Translocation of NF-kappaB and Promote Expression of the Anti-Inflammatory Cytokine Interleukin-10 by T Cells. Mol Cell Biol. 2018;38(22).
Balta E, Stopp J, Castelletti L, Kirchgessner H, Samstag Y, and Wabnitz GH. Qualitative and quantitative analysis of PMN/T-cell interactions by InFlow and super-resolution microscopy. Methods. 2017;112:25-38.
Wabnitz GH, Balta E, Schindler S, Kirchgessner H, Jahraus B, Meuer S, et al. The pro-oxidative drug WF-10 inhibits serial killing by primary human cytotoxic T-cells. Cell Death Discov. 2016;2(2):16057.
Baldauf, H.M., Pan, X. Erikson, E., Schmidt, S., Daddacha, W., Burggraf, M., Schenkova, K., Ambiel, I., Wabnitz, G., Gramberg, T., Panitz, S., Flory, E., Landau, N.R., Sertel, S., Rutsch, F., Lasitschka, F., Kim, B., König, R., Fackler, O.T., Keppler, O. SAMHD1 restricts HIV-1 infection in resting CD4(+) T cells. Nat. Med. 2012;18(11):1682-7.
Feldmeyer N*, Wabnitz G*, Leicht S, Luckner-Minden C, Schiller M, Franz T, et al. Arginine deficiency leads to impaired cofilin dephosphorylation in activated human T lymphocytes. International immunology. 2012;24(5):303-13. * equally distributed
Autenrieth SE, Warnke P, Wabnitz GH, Lucero Estrada C, Pasquevich KA, Drechsler D, et al. Depletion of dendritic cells enhances innate anti-bacterial host defense through modulation of phagocyte homeostasis. PLoS pathogens. 2012;8(2):e1002552.
Wabnitz GH, Goursot C, Jahraus B, Kirchgessner H, Hellwig A, Klemke M, et al. Mitochondrial translocation of oxidized cofilin induces caspase-independent necrotic-like programmed cell death of T cells. Cell death & disease. 2010;1:e58.
Klemke M*, Wabnitz GH*, Funke F, Funk B, Kirchgessner H, and Samstag Y. Oxidation of cofilin mediates T cell hyporesponsivenessunder oxidative stress conditions. Immunity. 2008;29(3):404-13. * equally distributed
Complete list
Group Leader
