Focus on neuroimmunology
Latest news
- We are delighted to welcome PD Dr Klemens Ruprecht. Klemens Ruprecht has been Head of the Neuroimmunology Section since 15 June 2025. He studied in Marburg, Berlin, Paris and London and obtained his doctorate in Berlin. After completing his specialist training at the Neurological University Hospital in Würzburg, he worked scientifically at the Institute of Virology, Saarland University Hospital, and then worked at the Department of Neurology at Charité - Universitätsmedizin Berlin as a senior physician, head of the MS outpatient clinic and research group leader. His clinical focus is on the diagnosis, differential diagnosis and treatment of inflammatory diseases of the CNS. Dr Ruprecht's scientific work focuses on the role of the Epstein-Barr virus in the pathogenesis of multiple sclerosis, CSF/serum biomarkers for inflammatory CNS diseases and neurovirological issues.
- The 11th MS Patient Day is currently being planned for January 2026.
Centre of gravity
The expertise of the neuroimmunology focus area is research into multiple sclerosis (MS) and autoantibody-associated diseases, in particular neuromyelitis optica spectrum disorders (NMOSD) and MOG antibody associated disorders (MOGAD) as well as autoimmune encephalitides and ataxias, paraneoplasia of the nervous system and myasthenia gravis. The focus here is on the transfer of basic science into everyday clinical practice within the framework of (inter)national, multi-centre studies for the development of new, targeted therapies. Our neuroimmunology outpatient clinic is certified by the German Multiple Sclerosis Society (DMSG) as a "recognised MS centre" and the associated cerebrospinal fluid laboratory by the German Society for Cerebrospinal Fluid Diagnostics and Clinical Neurochemistry (DGLN).
STRATEGY
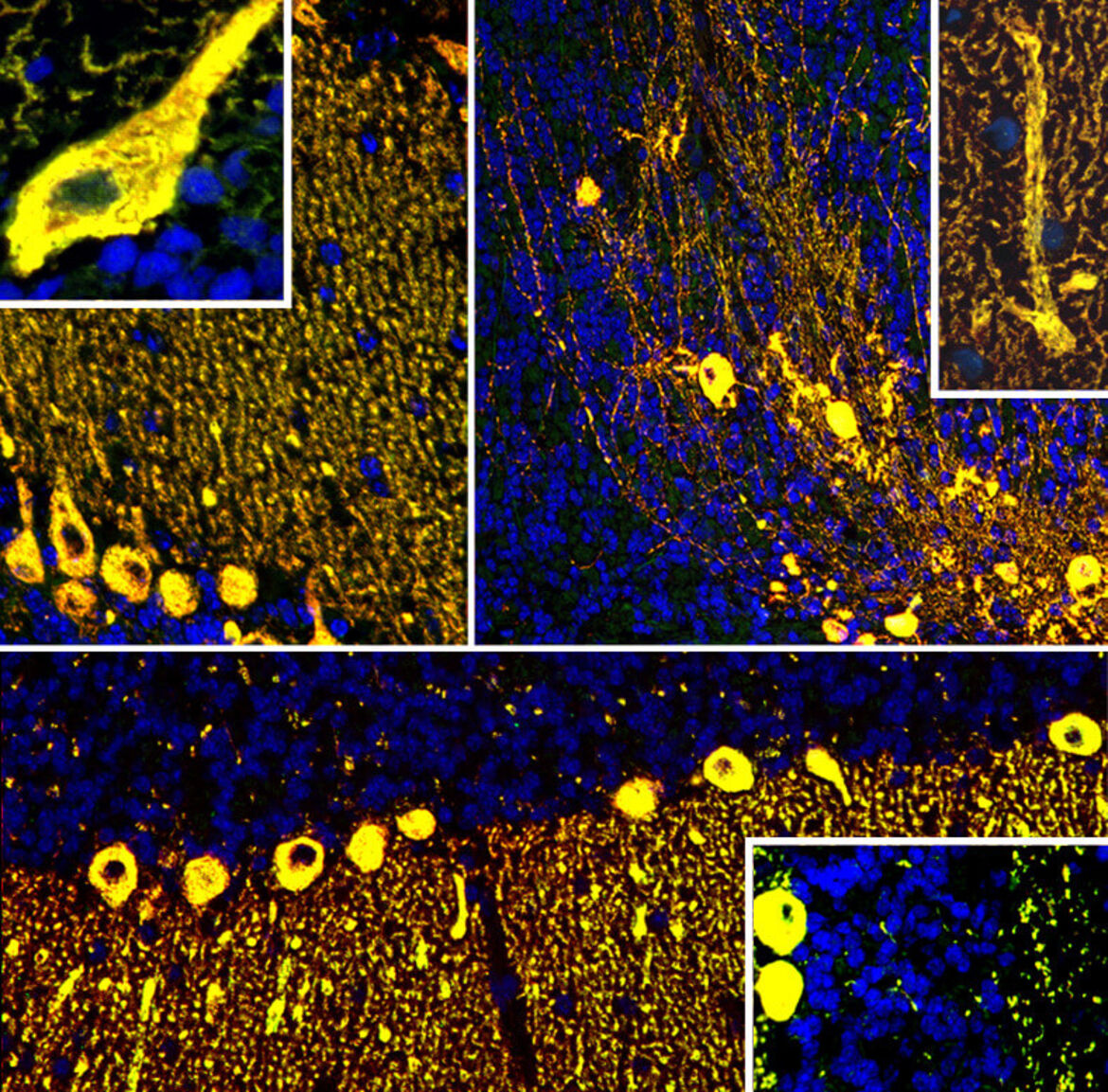
Clinical and experimental neuroimmunology/neuroinflammation is one of the five specialisations of the Department of Neurology alongside neurooncology, vascular neurology, neurological acute and intensive care medicine as well as degenerative diseases and movement disorders. The neuroimmunology/neuroinflammation focus - represented by the working group leaders Prof. Dr Brigitte Wildemann and Prof. Dr Ricarda Diem - aims to optimise the care of patients with neuroimmunological diseases by pooling clinical and scientific expertise as well as special expertise in cerebrospinal fluid diagnostics. In 2021/2022, > 1500 patients were treated in the outpatient/infusion outpatient clinic, often as part of clinical studies. The focus area works closely with the neighbouring clinical disciplines of neuroophthalmology, neurooncology, neuroradiology and neuropathology as well as the neurobiological working groups on campus. He spans the spectrum from animal studies on basic immunological and neurodegenerative mechanisms of MS and optic neuritis to human studies on mechanisms of immune regulation in MS and the pathophysiology of autoantibody-mediated diseases of the CNS (e.g. NMOSD], MOGAD, autoimmune encephalitides and autoimmune cerebellar ataxias), as well as serological, liquid analytical and imaging biomarkers in these diseases. With the help of this strategy, new diagnostic and therapeutic concepts are to be implemented directly in patient care. The Neuroimmunology Centre team attaches great importance to the rapid dissemination of new findings to colleagues (annual "MS Update" and "MS Patient Day", participation in the creation of important guidelines, numerous reviews and book contributions).
Goals
- Establishment of new therapeutic concepts for the treatment of chronic MS based on animal studies (calcium-mediated signalling)
- Establishment of new therapeutic procedures for the neuroprotective treatment of optic neuritis
- Rational selection of immunoactive and neuroprotective therapies from the growing portfolio of therapeutic options for MS based on suitable biomarkers
- Review of the benefit/side-effect profile of autologous haematopoietic stem cell transplantation (AHSZT) in MS using national cohorts
- Improving the diagnosis and treatment of NMOSD and MOGAD using large national cohorts and multicentre studies
- Identification of new autoantibody markers in patients with neuroimmunological diseases
- Characterisation of epigenetic markers with regard to female predisposition to neurological autoimmune diseases
- Identification of immunological mechanisms in patients with neuropsychiatric manifestations of post-COVID syndrome
OVERVIEW
The scientific activities of the programme include the analysis of basic mechanisms of the development of MS and optic neuritis in animal models (Fairless J Neurosci 2012; Lanz PNAS 2013; Hoffmann J Neuropathol Exp Neurol 2013, Bojcevski J Neurochem 2020, Fairless Invest Ophthalmol Vis Sci 2020, Schlüter Mol Ther Methods Clin Dev 2020, Fairless Front Neuroscience 2021, Boccuni & Fairless Life 2022, Richter Front Immunol 2021 2022, Fiedler J Neuroinflammation 2023, Boccuni, Neurobiol Dis 2023) and, as part of the BMBF-funded Clinical Competence Network Multiple Sclerosis (KKNMS), the investigation of basic immune cell dysfunctions in patients with MS (Haas J Immunol 2007, Haas J Autoimmun 2011, Schwarz J Immunol 2013, Balint Neurology 2013, Haas J Neuroimmunol 2016, Schwarz Neurol Neuroimmunol Neuroinflammation 2016, Haas Front Immunol 2019 2021) as well as the identification of new biomarkers under MS immunotherapy (Haas Mult Scler 2016), the establishment of new imaging parameters for monitoring the progression of optic neuritis (Laible PLos One 2016) and the implementation of investigator-initiated multicentre studies (Diem BMJ Open 2016, Lagrèze Lancet Neurol 2021, Küchlin Neurol Neuroimmunol Neuroinflammation 2023), the identification of new biomarkers in MS, autoimmune cerebellar ataxia and other immune-mediated diseases (Jarius Mult Scler J 2016, Jarius J Neurol 2016 2021 2022 2023, Jarius J Neuroinflammation 2016 2017 2018 2022, the characterisation of MOGAD as an independent entity including the diagnostic relevance of MOG-IgG (Jarius J Neuroinflammation 2016, Wildemann Acta Neuropathol 2020, Jarius J Neurol 2023), the characterisation of the CSF profile in MOGAD and neuro-COVID-19 (Jarius J Neuroinflammation 2016 2022) as well as overviews and consensus recommendations on NMOSD and MOGAD (Jarius Nat Rev Dis Primers 2021, Jarius J Neurol 2023, Kümpfel J Neurol 2024).
Funding includes the acquisition of the DFG Research Unit FOR2289 ("Calcium homeostasis in neuroinflammation and -degeneration: New targets for therapy of multiple sclerosis?") over two funding periods (start: end of 2015, spokesperson: Ricarda Diem, participation of Brigitte Wildemann in the second funding period), the acquisition of the BMBF-funded "investigator-initiated" multicentre study TONE(Treatmentof Optic Neuritiswith Erythropoietin, coordinators: Ricarda Diem, Heidelberg; Wolf Lagrèze, Freiburg), funding from the non-profit Hertie Foundation (MyLAb initiative, Ricarda Diem; multiple individual project funding, Brigitte Wildemann; msMED doctoral programme (Ricarda Diem, Brigitte Wildemann), also BMBF funding over 3 funding periods as a member of the Disease-Related Competence Network Multiple Sclerosis (KKNMS, Brigitte Wildemann), multiple grants from the Dietmar Hopp Foundation and Klaus Tschira Foundation for projects related to MS, NMOSD and MOGAD (Brigitte Wildemann) as well as funding from the Baden-Württemberg Ministry of Science, Research and the Arts for the Long COVID Alliance Heidelberg/Mannheim (Brigitte Wildemann).
The neuroimmunology focus, represented by Brigitte Wildemann's research group, is also one of the world's leading centres in the field of autoantibody-associated inflammatory diseases of the CNS, in particular NMOSD and MOGAD (Jarius and Wildemann Nat Rev Neurol 2010, Jarius J Neuroinflammation 2012, Jarius Brain Pathol 2013, Jarius J Neuroinflammation 2016, Jarius Nat Rev Dis Primers 2021, Jarius J Neurol 2023). In addition, the focus area also participates as a national coordinator (eculizumab in NMOSD, Michael Platten, Ricarda Diem) in multicentre therapy and cohort studies (SUSAC syndrome, Wildemann). As members of the KKNMS, the national NMO study group NEMOS and the International Panel for NMO Diagnosis (IPND), members of the working group were actively involved in the development of national guidelines for the diagnosis and treatment of MS and the international NMOSD diagnostic criteria. More recent focal points are the establishment of autologous haematopoietic stem cell transplantation (AHSZT) for the indication of MS and the elucidation of the pathophysiology of neurological manifestations of COVID-19 and long/post-COVID syndrome.